The III Symposium on the Effect of Chronic Hypoxia on Diseases at High Altitude
October 16-23, 2010
click here to go to the website
ABSTRACTS
BREATH-HOLD DIVING AND DECOMPRESSION SICKNESS.
Hans Christian Møller Thorsen, Poul-Erik Paulev & Gustavo Zubieta-Calleja
The Panum Institute, University of Copenhagen &
High Altitude Pathology Institute (IPPA), Zubieta University.
La Paz, Bolivia. www.altitudeclinic.com
Breath-hold diving is used in many parts of the world as a sport, in order to get pearls and as a record breaking activity. The Pearl divers in the South Pacific typically perform repetitive BH dives to depths of 30 m or more for 1.5–2.5 minutes for about 6 hours a day. Some of the divers developed what was called “Taravana,” a disease similar to DCS and suspected to be due to nitrogen accumulation. The divers who developed “Taravana” primarily were having symptoms from the central nervous system, including nausea, dizziness, and partial or complete hemiplegia. Paulev argued for a connection between DCS and BH diving (1965, 1967). Paulev himself and three other divers developed symptoms of DCS after a series of BH dives in a submarine escape-training tank in Norway. In each case, severe neurological symptoms and signs were present.
One of the objectives has been to develop a suitable computer model and calculate the amount of nitrogen—expressed as nitrogen tissue tensions—accumulated in the body during diving profiles.
Symmetric accumulation and elimination of an inert gas is described by a differential equation:
dII/dt = 0.693 ( Pamb.t – II)/T½
where II is the tissue pressure of the inert gas, Pamb is the ambient pressure at the actual depth and T½ is the half time period of the tissue. The differential equation is solved by numerical approximation:
II1 = II0 + 0.693 ( Pamb.t – II)/T½.
We have developed a dive table that may protect against decompression sickness, but its validity has to be evaluated in practice.
The danger is increased in mountain lake free diving, where breath-hold diving has not yet been practiced but will probably be done in the near future.
CHRONIC CONTINUOUS HYPOXIA INCREASES CARDIAC ISCHEMIC TOLERANCE VIA ACTIVATION OF MITOCHONDRIAL BKCa CHANNELS
Kolar F, Borchert GH, Neckar J, Ostadal B
Department of Developmental Cardiology, Institute of Physiology, Academy of Sciences of the Czech Republic, and Centre for Cardiovascular Research, Prague, Czech Republic
Chronic hypoxia increases cardiac tolerance against acute oxygen deprivation and its salutary effects persist for several weeks. Although several protective pathways have been identified, the mechanism of this long-lasting cardioprotective phenomenon is not fully understood. The aim of this study was to find out whether i) brief daily exposures to normoxia (reoxygenation) during the adaptation to hypoxia affects the induction of protected cardiac phenotype and ii) mitochondrial large conductance calcium-activated potassium channels (BKCa) contribute to its mechanism. Adult male Wistar rats were exposed to continuous normobaric hypoxia (CNH; FIO2 = 0.1) for 3–4 weeks; a subgroup of animals was allowed to recover at normoxia daily for a single 60-min period (CNH-R). CNH significantly reduced the size of myocardial infarction, induced by 20-min coronary artery occlusion and 3-h reperfusion, from 62% of the area at risk in normoxic controls to 42%. Protection by CNH was retained in subsequently isolated left ventricular cardiomyocytes subjected to 25-min metabolic inhibition followed by 30-min reenergization; it was detected as increased cell viability and reduced release of lactate dehydrogenase. These protective effects were completely absent in chronically hypoxic animals exposed to periodic reoxygenation (CNH-R). Pretreatment of cells with paxilline (BKCa channel blocker, 2 mM) significantly attenuated the improved resistance of cells from CNH rats without affecting normoxic controls. On the other hand, NS1619 (BKCa channel opener, 30 mM) protected cells from normoxic animals but no additional salutary effect occurred in the CNH group. However, myocytes isolated from CNH-R rats (that did not exhibit resistant phenotype) were protected by NS1619 similarly as normoxic controls. It is concluded that brief daily periods of normoxia during the adaptation to chronic hypoxia counteract the development of a cardioprotective mechanism which involves the activation of mitochondrial BKCa channels.
THE EFFECT OF PRENATAL HYPOXIA ON EXPRESSION OF TRX-1 AND LIPID PEROXIDATION PRODUCTS IN RAT HIPPOCAMPUS AT DIFFERENT PERIODS OF POSTNATAL ONTOGENESIS
Stroev S.A. 1,2, Tjulkova E.I. 2, Vataeva L.A. 2, Kislin M.S. 2, Samoilov M.O. 2, Pelto-Huikko M.T. 1
1 Tampere University Medical School, Tampere, Finland; 2 I.P. Pavlov Institute of Physiology RAS, St.Petersburg, Russia.
The effect of severe hypobaric hypoxia produced in a flow chamber (180 Torr, 3 times during 3 hours at 14th, 15th and 16th days of pregnancy) endured by pregnant Wistar rats on the thioredoxin-1 (Trx-1) expression was studied in hippocampal neurons of their descendants of the first generation at 3th, 14th and 80th-90th days of postnatal ontogenesis.
The expression of Trx-1 was studied in areas of cornu Ammonis-1, 2 and 3 (CA1, CA2, CA3) and dentate gyrus (DG) by immunocytochemistry that was assayed using two criteria: the total number of immunoreactive cells shown as a percent of control (Nt) and the number of intensely-labeled cells as a percent of control (Ni).
It was shown that hypoxia endured at the prenatal period significantly modifies the expression level of Trx-1 in hippocampal neurons of rats during their postnatal development. Herewith the direction of changes in Trx-1 expression may vary in different areas of the hippocampus and times of postnatal ontogenesis.
At the 3rd postnatal day in rats exposed to prenatal hypoxia, there was an statistically significant (P<0,05) decrease of Nt in CA1 (Nt = 74±9%) and Ni in CA2 (Ni = 47±13%) compared with the control rats of the same age. At the level of statistically non-significant but consistent trend (0,05<P<0,1) a reduction of Ni in CA1 (Ni = 60±8%) and increase Nt in DG (Nt = 122±4%) were also observed.
At the 14th day a statistically significant (P<0,01) decrease of Ni in the DG (Ni = 34±7%) and increase of Ni in the CA2 (Ni = 505±74%), were noted. At the level of trends (0,05<P<0,1) a decrease of Nt in CA1 (Nt = 79±7%) and increase of Nt in CA3 (Nt = 127±7%) were shown. Herewith the markers of lipid peroxidation level (Klein’s oxidation index, the level of diene and triene conjugates, thiobarbituric acid-reacting products (TBARP) and Schiff bases) were not perceptibly differ compared to control.
In adult age (80th – 90th days) a statistically significant decrease (P<0,01) of Nt in CA1 (Nt = 75±4%) and decrease (P<0,05) of Ni in CA3 (Ni = 43±17%) were noted. Nt in DG also tended to decrease (Nt = 84±7%; 0,05<P<0,1). Accordingly, the level of all lipid peroxidation products studied was markedly higher than in the controls.
These data suggest that severe hypoxia endured by maternal organism during the critical fetal development period, leads to a modification of pro- and antioxidant systems in hippocampal neurons of born rats throughout all their postnatal ontogenesis extending into adulthood. Along with the previously shown modifications of calcium and phosphoinositide systems of intracellular signal transduction, these changes reflect apparently one of the possible molecular mechanisms that underlie both adaptive and pathological modifications of cognitive and behavioral functions of animals exposed to prenatal hypoxia.
FOREVER: LOSS OF ADAPTATION, DOES NOT EXIST.
G Zubieta-Castillo & GR Zubieta-Calleja
High Altitude Pulmonary and Pathology Institute (IPPA), Zubieta University
La Paz, Bolivia.
zubieta@altitudeclinic.com
Chronic Mountain Sickness (CMS) is a term that does not explain the ethiopathogenesis of the disease in response to the effect of chronic hypoxia. There is no CMS, but rather pulmonary (mainly), cardiac, carotid, kidney, hematological or genetic disease. All these associated to an increase on the hematocrit or what is now known as polyerythrocythemia. CMS, was described by Carlos Monge Medrano close to 90 years ago. He was unable to find an explanation for the signs and symptoms and chose to use the term “LOSS OF ADAPTATION”. This was originally accepted, but today it can be appreciated as lacking significance. And should stop being used.
Undoubtedly, CMS is a chronic hypoxic process resulting in an increase of hemoglobin, due to pulmonary lesions (fundamentally), that alter the pulmonary function, thereby reducing the oxihemoglobin saturation and stimulating the increase of red blood cells. This, essentially occurs due to pulmonary lesions that are sequelae of diverse lung disease giving rise to intra-pulmonary shunts or uneven ventilation-perfusion. The term “LOSS OF ADAPTATION”, is even semantically inadequate, because in nature, living beings tend to adapt to different environments and circumstances. These could be: going to high altitude, temperature changes, solar radiation, UV radiation, diet changes, etc, etc . Consequently, to insist in contemporary medicine on the use of “LOSS OF ADAPTATION”, is not only a mistake, but rather foolishness!
The arterial oxygen content of blood in polyerythrocythemia, appears to be increased. However this apparent increase refers to the maximum oxygen carrying capacity of hemoglobin in blood when fully saturated. This gives rise to two conclusions:
1) that the hemoglobin in patients with polyerythrocythemia tends to be normal and is capable of full saturation when exposed to high oxygen pressures.
2) Fundamentally lung disease that results in intra-pulmonary shunts and uneven ventilation-perfusion, reduce the alveolar pressure of oxygen and the most efficient mechanism to compensate for this ventilatory deficiency is polyerythrocythemia.
The misunderstanding of these concepts has led to wrong interpretations of CMS such as “Loss of adaptation”.
Throughout history, all living beings, go through evolution, in order to adapt to different environmental conditions. Even aging is an evolution, that goes to finish a vital cycle. It never goes in the reverse way. This concept of loss of adaptation is unacceptable.
Again, “The organic systems of human beings and all other species tend to adapt to any environmental change and circumstance within an optimal period of time, and never tend towards regression (loss of adaptation), which would inevitably lead to death”.
ACID-BASE BALANCE AT HIGH ALTITUDES: A COMPREHENSIVE APPROACH USING THE MODIFIED VAN SLYKE EQUATION, TITRATABLE HYDROGEN ION DIFFERENCE (THID) AND OTHER ASPECTS.
G Zubieta-Calleja, PE Paulev, J Mehrishi* & G. Zubieta-Castillo.
High Altitude Pulmonary and Pathology Institute (IPPA), Zubieta University La Paz, Bolivia and *University of Cambridge, Cambridge, United Kingdom and The Cambridge Blood, Stem, Sperm Cells, Blood Doping and High Altitude Research.
The Acid-Base balance in the human body is calculated by the Van Slyke equation based on sea level measurements. The maintenance of blood pH within a fairly strict range at/around pH 7.4, with due consideration of the effect of hyperventilation, is essential for cellular function at any altitude. This is because various chemical processes occurring in the body, e.g., those involving proteins and enzymes, are pH-dependent. As is well known, oxygen and carbon dioxide partial pressures get lower as the altitude gets higher. At a permanent low production of CO2, the acid-base balance begins to change. Mountaineering physiologists, sadly, assumed that the sea level equation for A-B balance would be equally applicable, without any critical thought, and never thought of appropriate equations valid for high altitudes calculations. The Van Slyke equation for sea level seems to have been used indiscriminately for high altitudes in order to calculate for Base Excess (BE). It is essential to become aware that BE is an obsolete term and has been previously replaced by the concept of Titratable Hydrogen Ion Difference (THID).
For some extraordinary reasons, the BE equation without any critical discussion received the approval of CLSI for calculations of A-B balance at high altitudes (where the gas pressures are most certainly considerably lower). (CLSI:Clinical Laboratory Standards Institute, (http://www.clsi.org)).
The validity of the Van Slyke equation used for high altitudes, originally meant for sea level conditions, would clearly seem to be rather incongruous when critically considered. In our opinion it is not going too far to say that this procedure is woefully inadequate being inappropriate and to achieve excellence, is unacceptable. The higher the altitude the bigger the mistake in calculation of Acid-Base parameters.
Therefore, we took measurements and gathered information of the various parameters at high altitudes (2,500 3,500, 4,500m) to derive the urgently needed modified Van Slyke for quantifying Acid-Base balance at high altitudes. These are the key points and the thrust of our presentation. Consequently, we developed a modified Van Slyke equation for A-B balance and the adequate Ole Siggaard-Andersen nomograms adapted to different altitudes. We also discuss the point about the necessity of the adaptation factor according to the formula already developed and described in deriving the modified Van Slyke equation. The normal hemoglobin values for completely adapted individuals is likewise presented.
Acid-Base balance at any altitude can thus be adequately interpreted and, in fact, becomes crucial for the correct and precise interpretation of metabolic function. Furthermore, it is a life saving knowledge for mountaineers and high altitude residents around the world.
CLINICAL AND PROGNOSTIC VALUE OF INTERLEUKIN-12 IN PATIENTS WITH ACUTE MYOCARDIAL INFARCTION
Barbarash OL., Kashtalap VV., Zykov MV.
Research Institute for Complex Issues of Cardiovascular Diseases
Siberian Branch of the Russian Academy of Medical Sciences,
Kemerovo 650002, Russia
The research objective was to study clinical and prognostic value of inflammation markers in patients after Q-wave myocardial infarction (MI). The study enrolled 214 patients diagnosed with ST segment elevation MI. Cytokine levels (interleukins (IL)-1α,-6,-8,-10,-12 and tumor necrosis factor alpha (TNF – α)) were measured in all of the patients on days 10-14 after MI onset, and C-reactive protein (CRP) levels were detected by an immunoenzymatic method. Out of all analyzed inflammation factors only TNF – α, IL-12 and CRP were significantly higher in patients with multivessel coronary artery disease compared to patients with an isolated lesion. There was a positive correlation between the levels of inflammation markers IL-12 and IL-6 and the severity of an atherosclerotic lesion of brachiocephalic arteries or lower limb arteries. Data regression analysis with step-by-step selection showed the age of ≥ 53 years and IL-12 levels of ≥87,1 pg/ml to be of the greatest predictive value in detecting a haemodynamically significant coronary lesion, and the age ≥ 65 years and IL-12 levels of 108,8 pg/ml, in detecting a haemodynamically significant non-coronary lesion. II and > Killip class of acute heart failure and IL-12 levels of > 90 pg/ml were identified to be independent variables for risk stratification of any cardiovascular event a year after MI. Thus, out of all studied inflammation indicators IL-12 possesses the greatest diagnostic value in defining patients at a high risk of severe coronary and polyvascular atherosclerosis and subsequent complications.
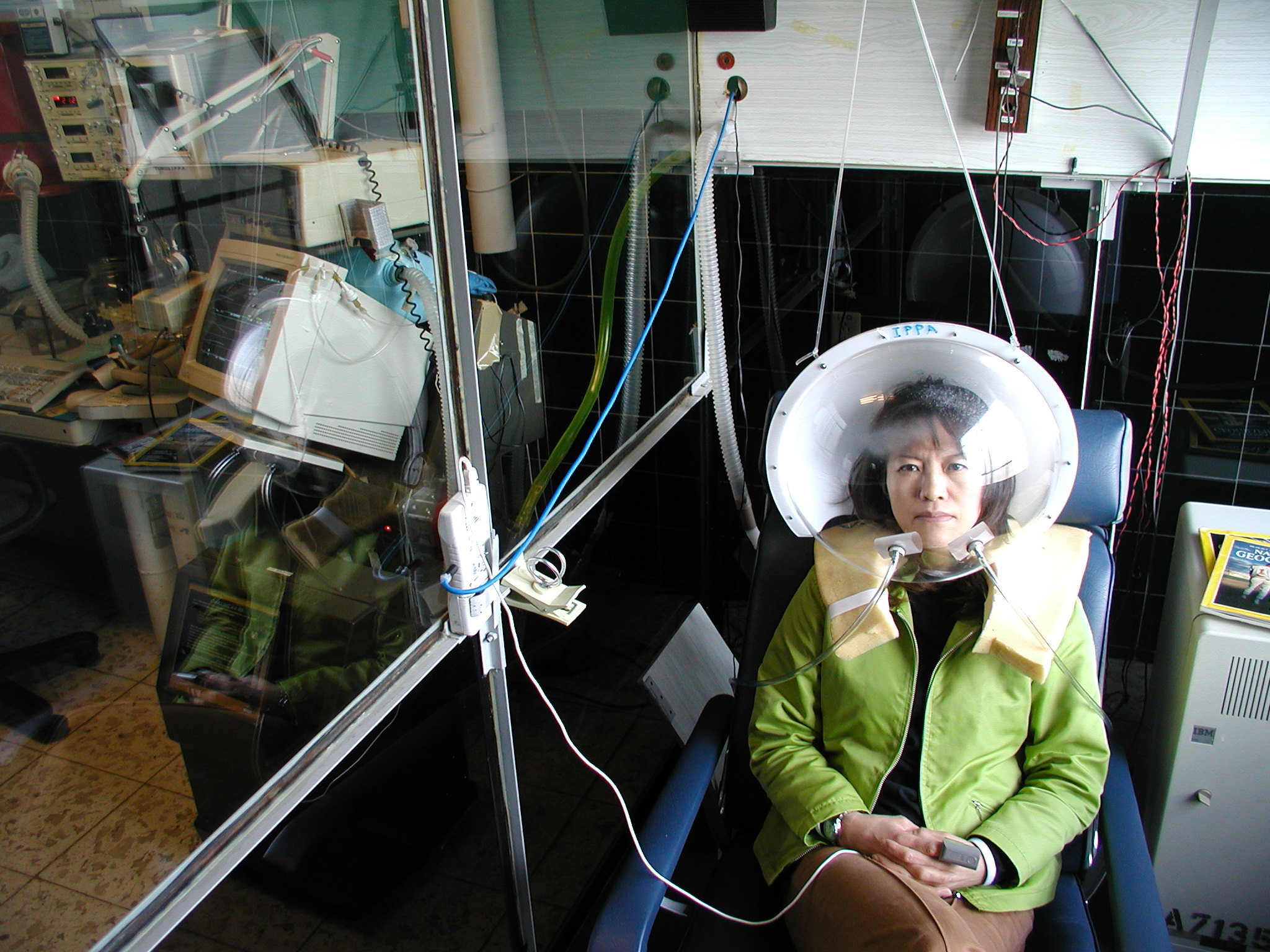
THE VENTILATORY HYPEROXIC SHUNT TEST AT 3510 m. OF ALTITUDE
L Zubieta-Calleja, G. Zubieta-Castillo & GR Zubieta-Calleja.
High Altitude Pathology Institute (IPPA), Zubieta University
La Paz, Bolivia.
www.altitudeclinic.com
We use a new method to test pulmonary shunt by hyperoxia at high altitude. The subject is tested first breathing ambient air in the seated position. Using a face mask, ventilation, ETO2, ETCO2, ECG, pulse oximetry and blood pressure are measured. An arterial blood sample is taken from the radial artery. The whole procedure is repeated with the subject breathing 100 % O2 from a Douglas Bag. This technique allows for precise measurements that provide a clear picture of cardio-respiratory parameters. Furthermore it allows the possibility of observing when there is an equilibration of the PIO2 as it is observed on a breath by breath basis in the same wave that the ETO2 is observed. The average PIO2 was 421.7 mmHg. For 3510 m, the altitude of our Laboratory, the test performed in 14 normal subjects(mean ± SD) using t-students reports:
|
SpO2 in % |
VE BTPS |
ETCO2 mmHg |
ETO2 mmHg |
PaO2
mmHg |
PaCO2 mmHg |
pH |
| Ambient Air |
91.56
± 1.45 |
9.19
± 2.3 |
28.05
± 1.9 |
66.42
± 4.05 |
59.3
± 5.92 |
27.7
± 3.72 |
7.43
± 0.03 |
| 89% O2 |
98.15
± 0.73 |
8.26
± 2.06 |
26.17
± 2.2 |
337.59
± 14.7 |
237
± 25.8 |
27.25
± 3.6 |
7.46
± 0.06 |
| p = |
<0.0001 |
NS |
<0.0001 |
<0.0001 |
<0.0001 |
NS |
NS |
This tests permits the operator to observe when the PIO2 reaches the maximum level thereby making the precise observation of shunt, irrespective of uneven ventilation that can delay such equilibration of inspired gases. The intra-pulmonary shunts are essential for evaluation of patients with Chronic Mountain Sickness at high altitude.
EXTREME HYPOXIA IN NEWCOMERS TO HIGH ALTITUDE, HOW CAN IT BE TOLERATED?
G. Ardaya-Zubieta, G Zubieta-Calleja, N. Zubieta-DeUrioste & GR Zubieta-Castillo.
High Altitude Pulmonary and Pathology Institute (IPPA), Zubieta University
La Paz, Bolivia.
zubieta@altitudeclinic.com
Patients suffering from the acute effects of hypobaric hypoxia can have extremely low arterial oxygen tensions (PaO2), which are quite well tolerated. They come to consultation with a PaO2 between 30 and 40 mmHg. Their recovery after a few days is uneventful following the efficient treatment of the underlying cause. When the medical reports were sent to their sea level physician they were asked: “Were you conscious?”
At sea level these very low oxygen tensions are not tolerable. A patient presenting a PaO2 of 60 mmHg is sent to an intensive care unit, as his life is in peril. However at high altitude in the city of La Paz 3600m, the normal acid-base values are: PaO2 = 60 ± 2 mmHg. PaCO2 = 30 ± 2 mmHg and pH = 7.40 ± 0.02, SpO2 = 91% ± 1%. The later oscillates with irregular breathing and deep breaths can achieve even 98% as has been previously described.
One out of four subjects, arriving to La Paz, has some form of Acute Mountain Sickness.
Some can present extreme hypoxia. The pathologies that we have recently seen associated with this extreme hypoxia are: pneumonia upon ascent, pulmonary thromboembolism, high altitude pulmonary or cerebral edema and several others.
As example a young Frenchman 25 years old climbed Huayna Potosi at 6000m two days after arriving to La Paz 3600 m, from Paris. On the way down he feels very short of breath. He is unable to sleep over the night. He comes to consultation walking. A blood gas analyses reports a PaO2 = 35 mmHg, PaCO2 = 29 mmHg and a pH = 7.53. This is diagnosed as severe hypoxia and respiratory alkalosis in High Altitude Pulmonary Edema. Would he have been alive if at sea level?
What is the explanation for this extreme hypoxia tolerance?
The alkaline pH during acute high altitude exposure shifts the oxygen dissociation curve to the left, allowing more capture and transport of oxygen. The other variable that can allow for the tolerance to extremely low PaO2 values is the normal low (relative to sea level) PaCO2. These new concepts are analyzed and discussed.
GERIATRICS AND EXERCISE AT HIGH ALTITUDE
OF Murillo, GR Zubieta-Calleja, G Zubieta-Castillo
High Altitude Pulmonary and Pathology Institute (IPPA), La Paz, Bolivia.
Hillside Internal Medicine, Hannover PA, USA
www.altitudeclinic.com
More and more, it becomes evident that exercise at sea level is essential, even for the elder. But at high altitude, there is little information on how much exercise can be performed by people above 65 years of age. At sea level, active 65 years old women have a life expectancy of 18.4 years compared to inactive at only 12.7 years. The NIH Consensus Conference on Physical Activity and Cardiovascular Health stated on exercise in the elder: “Benefits include reduction in mortality, reduction in symptoms, improvement in exercise tolerance and functional capacity, and improvement in quality of life”. Furthermore, several pathologies improve with exercise: elevated cholesterol, chronic lung disease, diabetes mellitus, high blood pressure, knee osteo-arthritis, obesity and osteoporosis. Exercise has been advised as being of two types by the American Geriatrics Society. 1) Vigorous = at least 20 minutes of vigorous physical activity on 3 or more days each week and 2) Moderate = a brisk walk, or an equivalently intense aerobic activity, for at least 10 min at a time, for a total of at least 30 min a day, on at least 5 days/wk. Vigorous exercise seems more benefitial, however it has to be achieved gradually and regularly in order to avoid injury. Exercise performed at 3510m in 4 normal people with ages ranging from 65 to 84 has shown that they have comparable SpO2, pulse and ventilation to young men in their early 20’s. The only difference is that 3 of the 4 subjects could not achieve the last stage of the USAF modified exercise protocol on a treadmill. Intensive exercise is limited in the elderly, but could be achieved gradually through training even at high altitude.
The guidelines for exercise in the elders at sea level
, are suitable for elders at high altitude. However, these should be gradually performed in newcomers and can reach full intensity of exercise, only when complete adaptation to high altitude is achieved from the hematological aspect.
THE HIGH ALTITUDE AND LOW ALTITUDE ADAPTATION STUDIES AND ITS PRACTICAL APPLICATION TO TRAVEL IN HUMAN EXPLORATION OF SPACE
G Zubieta-Calleja, N. Zubieta-DeUrioste & GR Zubieta-Castillo.
High Altitude Pathology Institute (IPPA), Zubieta University
La Paz, Bolivia.
zubieta@altitudeclinic.com
When sea level dwellers ascend to high altitude environments, their organism adapts in three phases to chronic hypoxia. Acute adaptation, that lasts between one and two days and where acute mountain sickness can occur. High Altitude Pulmonary Edema and high Altitude Cerebral Edema can likewise begin and extend towards the next phase. Subacute adaptation is the phase between the second day and the day total adaptation is achieved at a fixed altitude. The length depends on the time to reach the stable hematocrit and varies depending on the altitude. It is calculated using the formula:
Adaptation =
In this subacute phase if the subject performs excessive exercise, he feels short of breath, and the right heart can become dilated, and evolve to what is known as subacute heart disease. A consequence of incomplete adaptation. Finally, in the third stage when the hematocrit no longer increases, complete high altitude adaptation is achieved. Several factors, such as previous ascents, genetic characteristics, dehydration, quality of the food, presence of previous lung disease, and yet to be described factors, may alter somewhat the time frames. During full adaptation and life in the mountains, the subjects are able to carry out a normal life comparable to sea level, reproduce and practice sports.
Inversely, if high altitude residents go to sea level, the organism is facing a “relative hyperoxia” and hence, an aggression of an abnormal environment (disregarding the other factors such as temperature and humidity, food, lodging and so on). The hematocrit decreases linearly through neocytolysis and an abrupt stop of RBC production until a plateau is reached. Sometimes there is an over-boost taking the hematocrit to very low levels. This is attributed to a highly efficient use of oxygen.
The knowledge achieved herein is applied to a proposal for a most efficient capsule environment for the human exploration of Space. Currently space vehicles use sea level barometric pressure (760 mmHg) with normoxia (21%). Astronauts suffer, among many other complex micro-gravity alterations, anemia, that upon return to sea level, has to be correspondingly normalized to pre-flight levels. The reason that anemia presents is in part due to a lower requirement of oxygen by orthostatic muscles in Earth’s gravity. Consequently, a cabin pressure 2/3 that of sea level, similar to the city of La Paz, would maintain a hematocrit for re-entry, and furthermore, could significantly accelerate the preparation for Extra Vehicular Activity that currently takes up several hours, in order to avoid decompression sickness, going from a sea level pressure to 1/3.
AT 4000m IN THE HIGHLAND ENVIRONMENT, REMISSION OF SEA LEVEL LIFESTYLE RELATED DISEASE IS POSSIBLE THROUGH QUANTUM BIOLOGY
Prof.Kunihiro Seki., Dr.Antonio Saravia, and Prof.Takeo Nomura
Quantum Biology Institute, Japan
mail: seki822@yf7.so-net.ne.jp
In man, after the age of 20, cellular “redifferentiation” a form of cellular regeneration in 200 types of cells, with few exceptions will occur. But when you live at around 4000m, the altitude of Titicaca Lake, the dividing cells in the body undergo “transdifferentiation”. This would automatically be induced by cell division through drinking deuterium depleted water(DDW) and ingestion of deuterium depleted food(DDF) a consequence of low humidity and hypoxia.
The highlands at 3812m altitude in the mountainous regions of South America’s
Titicaca Lake, the UV radiation is 13 times that of sea level. At sea level, UV radiation increases the incidence of skin cancer by 3-6%. However at 4000m, high altitude residents – have apparently not suffered from skin cancer, however this needs to be further studied.
A subject was diagnosed suffering from a thyroid gland tumor at sea level. He migrated to La Paz Bolivia and stayed in the highlands at 4000m, and originally few physiological changes were observed. Until the arrival to La Paz, he had been ingesting DDW but no DDF. After 5 months, an ultrasonic diagnostic imaging practiced at the CiLap Hospital of La Paz reported remission and calcification of the tumor.
The validity of my hypothesis about the possibility of overcoming cancer by means of DDW and DDF was thus verified. An extraordinary achievement!
Life at the high altitude of 4000m as well as daily consumption of DDW and
DDF led to the multiplication of cells in the body, which resulted in such a reinforcement of cell proliferation, immune function and power of spontaneous cure that cancer remitted.
Going from the lowlands to highlands at 4000m above sea level, the following environmental changes and symptoms take place:
1 Partial pressure of oxygen at highlands is 120hPa which is 60% of lowlands (sea level PO2=206hPa).
2 Deuterium concentration of water and food is 138ppm while at sea level it is 150ppm.
3 The number of red blood cells increases by 1.6 times, and cardiopulmonary
function by 1.3 times and some men and women can suffer from nosebleed.
4 Cell proliferation becomes vigorous resulting in improved sexual health with
daily ejaculation for men and monthly ovulation for women.
5 With the improvement in the faculty of spontaneous healing, normally considered incurable diseases can have their symptoms temporarily alleviated or be completely cured.
Living at 4000m during one week (a diabetic’s?) fasting glucose levels reported 100mg/dl. This is evidence that insulin has proliferating β cells that secrete insulin in the pancreas islet. Upon returning from 4000m to sea level, these conditions remained for a month. At 4000m, the altitude hypoxic environment with low temperature and dry air is a spontaneous cure and improves immune function and metabolism in type 2 diabetes-affected people at sea level.
In conclusion, quantum biology supplies a theoretical basis for the remission of cancer
which has been considered incurable.
1. In people exposed to high altitude hypoxia, low atmospheric pressure, low temperature and dry air, immediately stimulates cell division in their body enhancing cell proliferation, immune function becoming a power of spontaneous cure.
2. If one consumes DDW and DDF available at the altitude of 4000m above sea level, cell proliferation, immune function and power of spontaneous cure are all strengthened.
3. Healthy sexual life activates cell proliferation, immune function and power of spontaneous cure.
When all three above-mentioned conditions are met concurrently, owing to their synergistic effect, cancer in the human body can go into remission.
SIR CHRISTIAN JOHN STOREY BONINGTON
Interview by Jay Mehrishi
Cambridge University, UK
Sir Christian John Storey Bonington, CVO, CBE, DL (styles himself as ‘Chris’ Bonigton) is a British mountaineer, born on August 6th, 1934 in Hampstead, an area of London, 4 miles (6.4 km) north-west of Charing Cross rail station. He was educated at University College School in Hampstead, London and joined the Royal Fusiliers before attending Royal Military Academy Sandhurst. On graduation, in 1956 he was commissioned in the Royal Tank Regiment. After three years in Northern Germany, he spent two years at the Army Outward Bound School as a mountaineering instructor.
He is married to Wendy, who is a freelance illustrator of children’s books. The couple have two sons: Daniel and Rupert.
Following a request by Larry Silver (from California) to say a few words to the conference that arrived while he happened to be in Cambridge for delivering a lecture elsewhere, he kindly invited me to a breakfast meeting on Sep 23rd and an interview. It was an immense pleasure for me to meet Sir Chris Bonington in the courtyard of Corpus Christi College under the typical light English rain falling on us!
At breakfast he had 2 rashes of bacon and a sausage (can’t remember if he had any fried egg), grilled tomatoes, orange juice and a slice of toast (that he did not eat). Looking at my one tablet of weetabix, grilled tomatoe and some basked beans, he remarked on the type and small size of the breakfast.We had a most interesting discussion in the rooms after we both fiddled with the simple tripod mechanics, the digital camcorder that I had not used for four years and of course, the rather poor light. Like a true experienced mountaineer taking things in his stride, Chris thought that the natural light would be fine and we got on. Fortunately, he had the same Apple Laptop as mine, that had all the questions I was asked by Gustavo and Larry to put to Chris.
Amongst other things about AMS, nausea, fatigue, rate of climb, adaptation (that he thinks varies from person to person), in particular, Chris recalled about the blood getting ‘thicker’. In a sentence I described to him how oxygen getting rarer, the need for more oxygen, requests more Hb and thus more RBCs, triggered by EPO to make more RBCs! He surprised me by the extraordinary story of a climber’s hematocrit remarkably reaching as high ~70% and the attending physical having to remove 2 litres of blood ( that he, otherwise, believed, would have died) and administer saline!Because of my interests since 1960 in the viscosities of human blood in cardiovascular disease and red cell mass increase in climbers at high altitudes, I found this of particular interest.
At the end of the interview, he finally packed his roller bag and we walked for 4 min to my car for the 10 min drive to the rail station to catch the train to London and his home in Cumbria. We talked a little in the car about various things.Like any proud grandfather he showed me the photographs of his grand children and of course he asked me about my family.
His career has included nineteen expeditions to the Himalayas, including four to Mount Everest and the Bonington was part of the party that made the first British ascent of the South West Pillar of the Aiguille du Dru in 1958, and the first ascent of the Central Pillar of Freney on the south side of Mont Blanc in 1961 with Don Whillans, Ian Clough and Jan Dlugosz. In 1960 he was part of the successful joint the British-Indian-Nepalese forces expedition to Annapurna II. On leaving the British Army in 1961, he joined Van den Berghs, a division of Unilever. But he left after nine months, and became a professional mountaineer and explorer. In 1966 he was given his first assignment by the Daily Telegraph magazine to cover other expeditions, including – climbing Sangay in Ecuador; hunting Caribou with Eskimos on Baffin Island. In 1968 he accompanied Captain John Blashford-Snell and his British Army team in the attempt to make the first ever descent of the Blue Nile.
He has written fifteen books, made many television appearances, and received many honours, including, since January 2005, the chancelloship of Lancaster University.
He is honorary president of the Hiking Club and Lancaster University Mountaineering Club and has a boat named after him among Lancaster University Boat Club’s fleet. Furthermore he is the Honorary President of the British Orienteering Federation. He has lived in Cumbria with his wife, Wendy since 1974. He is a patron, and former president (1988-91), of the British Mountaineering Council (BMC). He succeeded Sir Edmund Hillary as the Honorary President of Mountain Wilderness, an international NGO dedicated to the worldwide protection of mountains. Noteworthy:
1970 Annapurna (south face), successful, summit reached by Haston and Whillans death of Ian Clough
1972 Mount Everest, (south-west face), unsuccessful
1975 Mount Everest (south-west face), successful, summit reached by Scott, Haston, Boardman, Pertemba Sherpa and Mick Burke; death of Burke
1978 K2 (west face), unsuccessful; death of Nick Escourt
1982 Mount Everest (north-east ridge), unsuccessful; death of Boardman and Tasker
Parts of this description has made use of the biography of Sir Chris Bonington on the
Website http://en.wikipedia.org/wiki/Chris_Bonington that is duly acknowledged and Sir Chris Bonington also will have been consulted for the accuracy for which the writer Jay Mehrishi, the Director of High Altitude Pulmonary and Pathology Institute IPPA (Gustavo Zubieta-Calleja), the Chairman of the III Symposium on Chronic Hypoxia (Gustavo Zubieta-Castillo) and the President of International Society of Chronic Hypoxia ISCH, (Larry Silver) are thankful.

 Furthermore, you can easily imagine, the outstanding world exposure this will generate, a true leading edge future scientific trend!
Furthermore, you can easily imagine, the outstanding world exposure this will generate, a true leading edge future scientific trend!




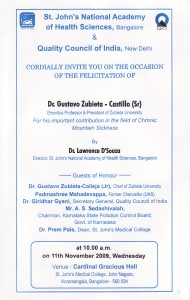 Upon returning to Bangalore Prof. Zubieta-Castillo (Sr.) and Prof. Zubieta-Calleja (Jr.) were invited to give a talk at the St. John’s Medical College (see the invitation on the left). Much to their surprise, Prof. Thuppil Venkatesh leaded in the presentation and introduced the Director of the St John’s National Academy of Health Sciences Dr. Lawrence D’Souza, along with very distinguished personalities of Bangalore.
Upon returning to Bangalore Prof. Zubieta-Castillo (Sr.) and Prof. Zubieta-Calleja (Jr.) were invited to give a talk at the St. John’s Medical College (see the invitation on the left). Much to their surprise, Prof. Thuppil Venkatesh leaded in the presentation and introduced the Director of the St John’s National Academy of Health Sciences Dr. Lawrence D’Souza, along with very distinguished personalities of Bangalore.

 With Prof. Thuppil Venkatesh, Principal Advisor Quality Council of India (QCI) &
With Prof. Thuppil Venkatesh, Principal Advisor Quality Council of India (QCI) &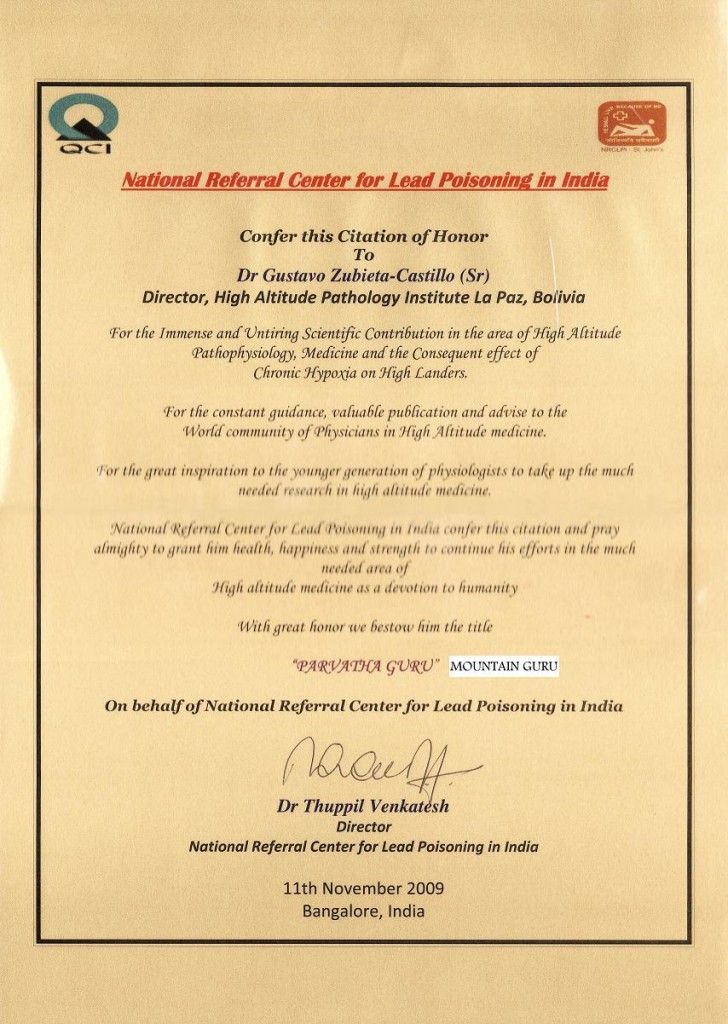
 Shown here Shashidhara N, Gustavo Zubieta-Calleja (Jr), His excellency Governor of Karnataka H R Bhardwaj, Gustavo Zubieta-Castillo (Sr), Thuppil Venkatesh.
Shown here Shashidhara N, Gustavo Zubieta-Calleja (Jr), His excellency Governor of Karnataka H R Bhardwaj, Gustavo Zubieta-Castillo (Sr), Thuppil Venkatesh.