CONSENSUS STATEMENT by and Ad Hoc Committee of the International Society for Mountain Medicine on CHRONIC HIGH ALTITUDE DISEASES
Xining, August 2004
These guidelines are established to inform the medical services onsite, who are directed to solve high altitude health problems, about the definition, diagnosis, treatment and prevention of the most common high altitude diseases. The health problems associated with life at high altitude are well documented, but health policies and procedures often do not reflect current state-of-art knowledge. Most of the cases of high altitude diseases are preventable if onsite personnel identify the condition and implement appropriate care.
This consensus statement has been developed by medical/scientific experts from the Committee experienced in the recognition and prevention of high altitude diseases.
Affiliations of the Ad Hoc Committee on Chronic High Altitude Diseases
Co-Chairs : Fabiola León-Velarde (UPCH, ISMM and ARPE, Perú) and
John T. Reeves (……., USA).
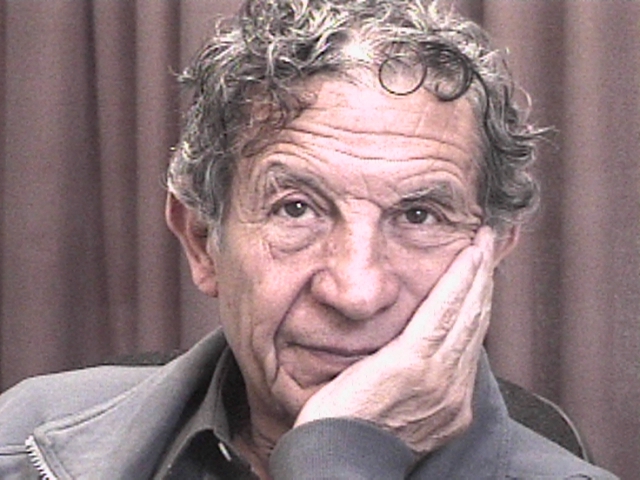
Committee : Almaz Aldashev (…….,, Kyrgyz Republic) ; Ingrid Asmus (……. ; USA) ; Luciano Bernardi (…….., Italy) ; Ri-Li Ge (……, China); Peter Hackett (ISMM and WMS, USA); Toshio Kobayashi (…….., Japan) ; Marco Maggiorini (…….., Switzerland); Lorna G. Moore (ISMM, USA) ; Dante Peñaloza (UPCH, Perú) ; Jean Paul Richalet (ISMM and ARPE, France); Robert Roach (ISMM, USA); Tianyi Wu (…….., China) ; Enrique Vargas (ISMM and IBBA, Bolivia) ; Gustavo Zubieta-Castillo, Sr., ; Gustavo Zubieta-Calleja, Jr. (ISMM, IPPA, Bolivia)
At this point, the Zubieta draft (click here) for the final version to be defined in Xining, China, was sent by us.
At Xining we were mostly ignored with our concepts, where we were the ones actually diagnosing and treating these patients in the cities of La Paz, and El Alto, Bolivia between 3,100 to 4,100m of altitude.
The final version of the Consensus Statement on Chronic and Subacute High Altitude Diseases can be found here.
It becomes clearly evident that of all the references we provided, only one was included. The rest were totally droped out.
This meant a great loss for the high altitude health systems around the world, since 2005 (16 years as of 2021 when this article was writen).
We did achieve that the term “Loss of Adaptation” be dropped but it continues to be used regularly as of 2021.
Nevertheless, it was during this time that we received an email that Prof. Dr. Gustavo Zubieta-Castillo responded after some time as a public letter entitle “FOREVER, LOSS OF ADAPTATION DOES NOT EXIST“